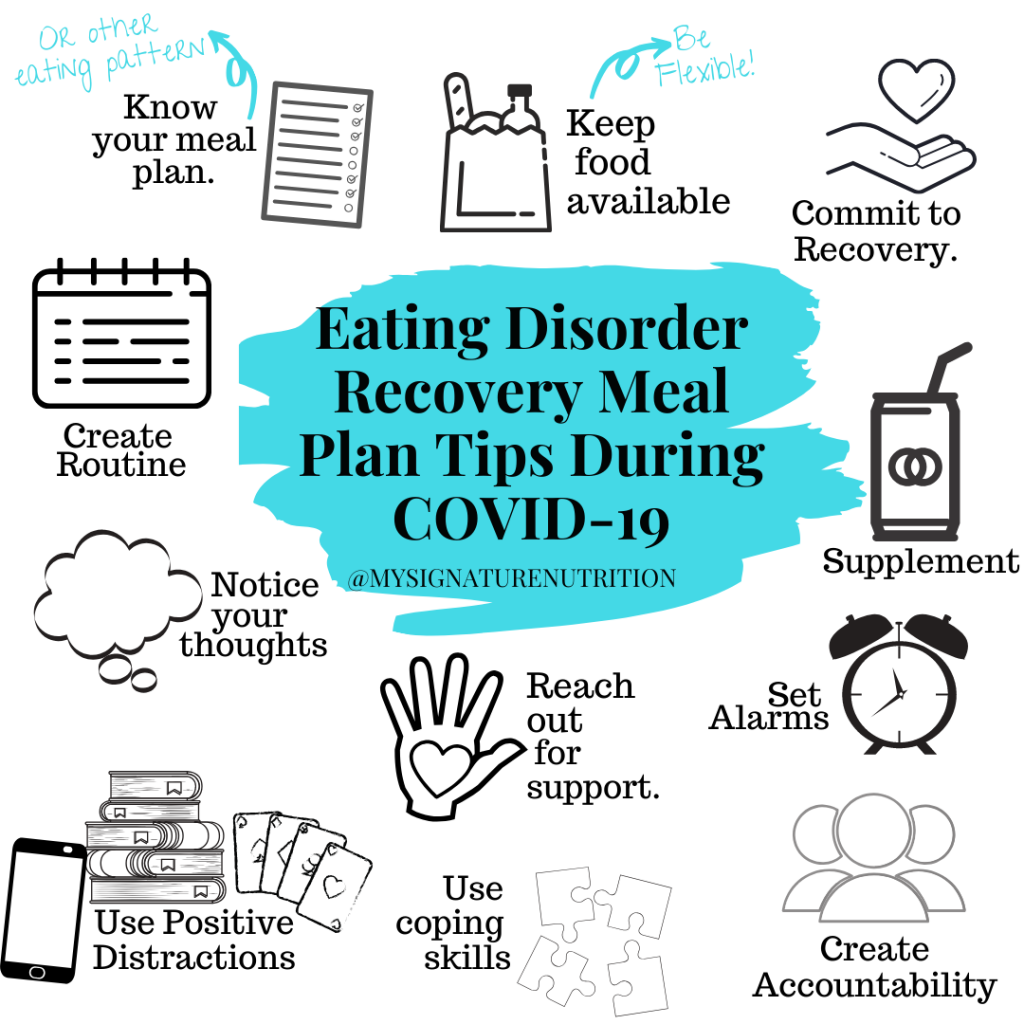
11 Tips to Support Consistent Eating (for eating disorder recovery) During COVID-19 (or another stressful event)…
March 23rd, 2020 by Sara Upson
Eating disorder recovery is hard. There’s no way around it. IT just is.
It’s hard enough to recover during “normal” times.
And now here we are in unprecedented times and there are still so many brave ones continuing to work on their recovery. I see you.
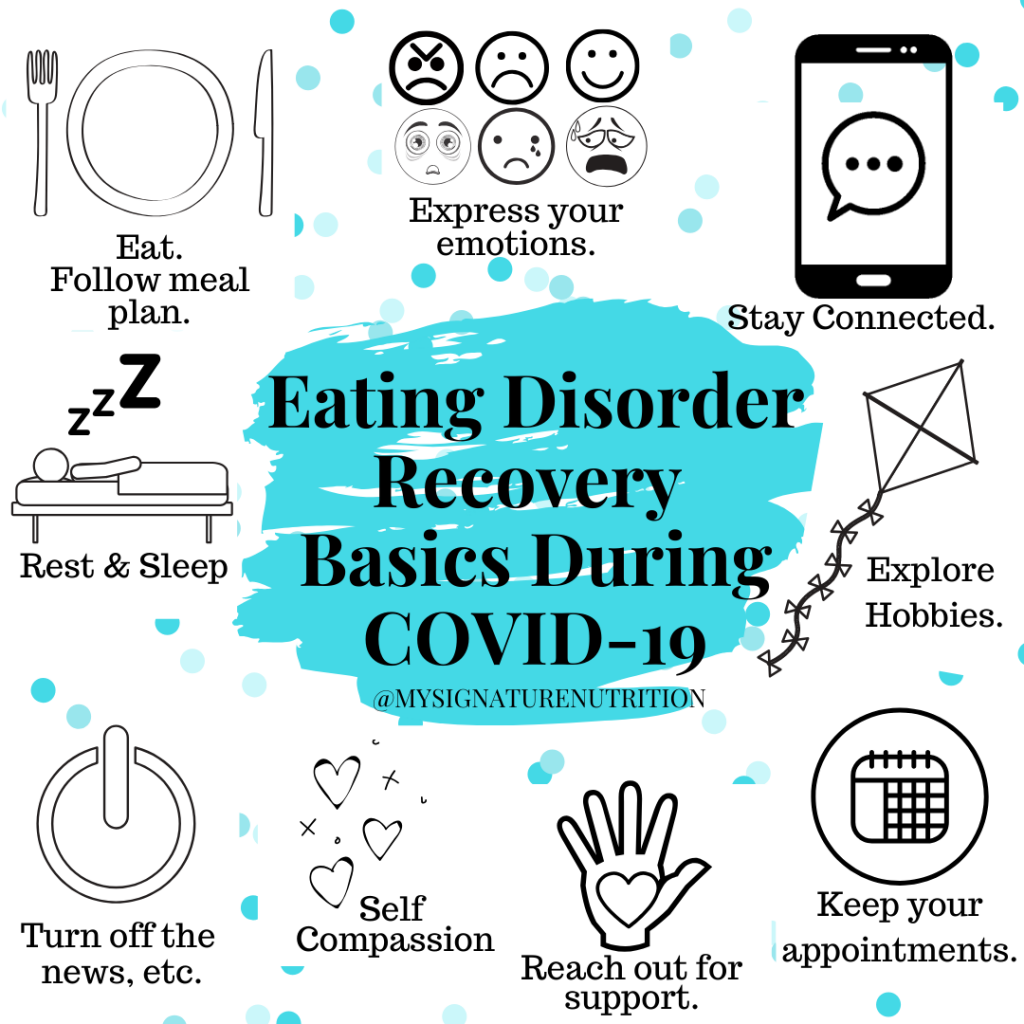
A recent post I shared on Social media discussed ED recovery tips for during COVID-19 pandemic. I had a few people DM me with specific questions and concerns- and most all focused on meal plan:
-I’m struggling to follow meal plan.
-If only it was that easy to follow meal plan.
-I feel so overwhelmed, meal plan is hard.
-Lack of food availability increases my urges to restrict meal plan.
If you’re struggling with meal plan (or consistent eating) too, you’re not alone. Meal plan is an essential part of recovery for many people and it’s hard. To support you with following meal plan, at any time, but especially at this stressful time, here are some tips and ideas.
< If you’re not on a meal plan, but working to heal your relationship with food many of these are still relative and supportive for you as well. >
1. Know your meal plan. For most people, this isn’t a problem, however changes or updates sometimes get left off. Or maybe you haven’t used meal plan for awhile (you’ve been transitioning to body cues) but you’re struggling and need to return to meal plan for more structure or support. Wherever you are in the process it’s essential for you to know your meal plan. I’m not saying that you have to hang it on your fridge- but you could- if that’s supportive to you. If not, make sure you have it somewhere you can reference. And the stick to it.
If you don’t have a meal plan, then know your routine for consistent eating and that you’ll commit to getting enough food in to nourish your body and support recovery.
2. Keep food available. It’s hard to follow your meal plan if you don’t have all the items that you need. Now I know you might think, but I can’t access all the food that I need. This is where it’s important to think flexibly. A grain is a grain, a protein is a protein, a fat is a fat, etc. Perhaps you can’t get the one you want, the one that feels safe, the one that your eating disorder likes more- but you can get something.
You can keep food on hand so that you can make sure that you’re able to follow plan. If the grocery store is difficult there are many, many options now to shop online, via an app and pick up food or have it delivered. This is even something you can do with your dietitian in session if you need support.
If you’re struggling with food insecurity please reach out to your foodbank, salvation army, local churches, or within the community to learn about options available to help support you. You have to eat and to do that you must have food.
3. Commit to Recovery– I’m fully aware that this is easier said than done. However, you can commit to keeping your focus on recovery. Yes life might keep pulling you away, but you can keep bringing your attention back to what you need to do next. AA talks about doing the next right thing. In her book Life Without Ed Jenni Schafer talks about no matter what or whatever it takes. However you want to think about it, it’s important to keep committing to your recovery and following your plan. It’s not permission to get off plan, but permission to not beat yourself up and then to focus on getting right back on plan.
Additionally if you’re able to fully throw yourself into recovery and commit to follow meal plan, no matter what- then it can actually help to reduce anxiety about meal plan. How? Because then, not every meal, snack or exchange will be a question of if, when, or whether you’ll have it. You’ll already know. Yes, you’re having it and you’ll figure out how to get it in. Commit.
4. Create a routine. Include meals and snacks (aka meal plan or your eating pattern) as part of that routine. When eating and following meal plan is just part of what you do every day it is so much easier to keep with it. Of course this can be thrown off by work and life in general- but creating and sticking to a routine can be so helpful. The routine could be based on certain times of day, when you wake up, other events that you do throughout the day, etc. Sometimes even the act of eating may be the thing that anchors you to your day and creates routine and that’s okay.
5. Set Alarms. If you use recovery record you’re likely already getting multiple text reminders throughout the day to remind you to eat and or log food. Sometimes even those can get old though and you can silence them pretty quickly from your phone. Sometimes you may need an actual alarm to go off that you have to turn off and sometimes you may need a backup alarm. You may not need the alarm for all meals or snacks so you can set it for whenever you need more support.
The alarm won’t be magical and make you eat- but it will bring your attention to the fact that it’s time to eat. Additionally, if it’s time to eat and you choose not to eat-that’s useful information to take into your dietitian and therapist. It’s also useful information for you to consider what is getting in the way of your eating, why is that?
6. Create accountability. If you have a dietitian or treatment team- this may be with them. It could also be a recovery coach, friend, family member, significant other, loved one or someone you connect with online. Let them know that you’ve eaten or that your struggling. Also remember that when you aren’t able to follow plan you’ll be held accountable and asked why. This isn’t punitive but to help support you in recovery.
7. Reach out for support. Again, this could be any of the individuals listed above. And it could include reaching out before, during or after eating. Or any time really. Maybe just when thoughts present. Whatever it is- as you have urges or thoughts about not following meal plan/eating- reach out for support. As you prep or have desires to not eat- reach out or support. Then remember that commitment.
8. Distraction & Use coping skills. Sometimes checking in with emotions is helpful with following meal plan. Sometimes it’s not. You don’t need to eat every meal mindfully and if you’re in early recovery I don’t recommend mindful eating. It’s too much. If you’re already feeling too much, the world feels like too much, then I guarantee your food will feel like too much. It’s not. What you need is to eat and nourish your body. If the only way you can do that is with distraction, that’s okay.
Do whatever you need to do to nourish your body and get food in: TV, games, music, read, social media, facetime, talk on the phone, color, whatever works for you! It’s okay to distract yourself or use other coping skills to make sure that you’re following meal plan. Other coping skills that might be helpful here are opposite action, aligning with your values, grounding, deep breathing, defusion, prayer or meditation, or self-compassion (just to name a few).
9. Notice your thoughts. When you’re struggling with meal plan, notice your thoughts about meal plan, eating, and body image. Notice what you’re saying, when you say it and the words you use.
It will probably be overwhelming to do this all the time, especially in the beginning. Notice it most when you find yourself resistant to eating or unable to follow meal plan.
Check in with yourself to ask what am I feeling, what are the thoughts behind those feelings? What is going on that I feel like I can’t eat? What would I need to be able to eat? The words you choose and the thoughts you have are not random. They are specific and can communicate so much. Take them to your dietitian and therapy sessions and learn how to interpret them yourself so that you can get what you really need. It will feel like you need to use a behavior, but what you really need is to eat and eat consistently. No matter what.
10. Supplement. No one really likes to supplement and it certainly takes a lot of commitment, but if you aren’t able to get food in or finish meal plan- then commit to supplementing. To supplement whatever you’re not able to finish or whatever you don’t have. Yes, it’s hard- and you can do it!
While I would love you to do all of these, I also recognize that they might not all be possible. Here are some ideas to get started:
- Check in with yourself on a scale of 1-10 for each one with 10 being 100% possible and 1 being not likely at all. Then follow up by asking yourself where you could start.
- Check in and ask yourself what you would need to move numbers up on each scale of do-ability. Then pick one to two things that you can commit doing.
- Try to grow that list each couple days-weeks.
Your eating disorder won’t like it and it will feel hard, but it will help you move forward during this difficult time. Sending you so much love and compassion. 💗
Comments are closed.